The Health Insurance Portability and Accountability Act (HIPAA) enforces how you must retain and protect sensitive user data in a healthcare setting. Compliance is mandatory, and knowingly breaching HIPAA rules (including disclosing health information of individuals) comes with hefty fines and even jail time. It is important that your data practices and infrastructure and the third parties you trust to store and protect sensitive information, recognize and comply with HIPAA regulations.
This article will help you better understand HIPAA data backup requirements in regard to archiving and data backups (including encryption and offsite backups), and explains the HIPAA Security Rule so that you are aware of your responsibilities and how to remain in compliance with regulation.
Importance of data backup in healthcare
Data backup is vital to the ongoing operation of any organization and is especially important in healthcare: information needs to be retained for ensuring the ongoing health of patients (for example, reviewing their medical history), as well as for potential legal requirements (like reviewing historical internal communications).
Healthcare information is also highly personal and sensitive, and it is your responsibility to protect the privacy of those who have trusted you with it and treat it with care by providing proper oversight to prevent it from being exposed or shared without consent.
Because of this, you must implement backup policies and infrastructure that is both robust and fully HIPAA compliant.
Understanding HIPAA data backup requirements and the HIPAA Security Rule
Before you can understand your HIPAA obligations, you need to determine whether you are a covered entity or business associate that deals with ePHI, as defined below:
- ePHI (Electronic protected health information) is any digitally stored or transmitted information regarding a person’s health or healthcare that they have received, including notes, lab results, and billing and insurance information.
- Covered entities refer to any parties who handle ePHI and are required to comply with HIPAA regulation — this includes everything from organizations such as hospitals, pharmacies, and nursing homes to doctors, chiropractors, and psychologists.
- Business associates are parties that provide services that handle ePHI to covered entities or other business associates, such as IT service providers, cloud platforms, and consultancies.
Healthcare data that you are obligated to retain and protect will depend on what your organization does and may include records of policies, procedures, staff training, complaints, security incidents, access and audit logs, risk assessments, and electronic communications.
Additionally, agreements and records regarding relationships between covered entities and business associates must also be stored. HIPAA specifies that these be retained for 6 years; however, various state and local laws may enforce data retention of data relating to healthcare for longer periods, sometimes up to 10 years.
If you are a covered entity or business associate handling ePHI, you must comply with the relevant HIPAA regulations. Under the HIPAA Security Rule, your responsibilities for the data that you retain and backup include:
- Ensuring the confidentiality of all ePHI that is created, maintained, received, or otherwise transmitted.
- Maintain the integrity of all ePHI against alteration, corruption, or deletion.
- Provide reasonable protection against anticipated threats to the security of ePHI.
- Protecting against unauthorized access and misuse of data.
- Ensure that staff and other parties granted access to ePHI are themselves compliant.
In addition to the HIPAA Security Rule, if you are storing or backing up ePHI using services provided by third parties, you must be aware of the associated Privacy Rule for sharing health information. The HIPAA Privacy Rule defines a patient’s rights to access and amend their ePHI, as well as laying out the requirements for covered entities and business associates in regard to disclosing how data is used and shared, and if an unintended disclosure or breach occurs.
Once you’ve planned your data backup practices, hardware, and services, you should carefully review the official HIPAA documents, as well as any other regional regulatory requirements that you need to meet surrounding healthcare and user privacy.
Implementing HIPAA-compliant data backup procedures
In addition to stipulating what data should be retained, HIPAA also specifies data storage and backup standards and requirements for maintaining the integrity and availability of ePHI.
When implementing data solutions that handle healthcare information, you should ensure that you include the following:
- Data backup and disaster recovery plans: These should include the regular testing and maintenance of your backup apparatus, including verifying the integrity of backed up data (i.e. that an exact copy has been made) and offsite backups so that data can be restored in the event of a disaster. Restoration processes should be regularly tested.
- Emergency mode operation plan: ePHI should be available even in the event of an emergency (including natural disasters, security incident, or theft), utilizing offsite backups and redundant systems to ensure continued access to health data is possible.
- Testing and revision procedures: In addition to regularly testing your data systems and the integrity of the data itself, you should regularly run and test the effectiveness of data backup and disaster recovery plans and revise them to meet new requirements or changes.
- Application and data criticality analysis: Prioritize the backup of essential systems and regularly test the effectiveness of recovery processes.
Your data policies and plans, along with the audit logs for them, should also be included in your HIPAA-compliant data backups to ensure compliance and accountability.
Backup best practices and additional security measures
When implementing your data backup infrastructure for healthcare use-cases in the United States, you should ensure to follow best practices by following standard redundancy and security and encryption measures:
- Scheduled, regular backups: Ensure that backups are run automatically on a schedule and regularly enough that changes to ePHI are effectively captured. This may require different backup schedules for frequently changing data.
- Manual backups: You should be able to readily perform manual backups when requested or when a major system change or software update is to be undertaken.
- Multiple offsite backups: You should ensure up-to-date backups are stored offsite in case local copies of data are destroyed in a disaster scenario. This should comply with your data backup and disaster recovery plan, and should include backups stored in the cloud as well as backups stored on physical media that you remain in full control of. A minimum of three copies of data is recommended.
- Data encryption: All backed up ePHI should be encrypted during transit and at rest to ensure HIPAA compliance.
- Access control: Restrict access to data and backups to only those authorized to work with it. Role-based access control (RBAC) is an effective model for managing access to sensitive resources. Two-factor authentication should also be implemented to protect data infrastructure from unauthorized access.
- Physical security: Physical access to devices containing sensitive healthcare data should also be restricted.
- Firewall and endpoint protection: Protect your network with strict firewall rules and deploy endpoint protection to your devices to help prevent cyberattacks and malware.
- Education and communication: Team members should be aware of their responsibilities surrounding data privacy and security and feel confident in alerting stakeholders to potential data loss or misuse so that appropriate mitigation and recovery measures can be taken.
You should also thoroughly document and regularly perform security audits on your entire IT apparatus (including staff and contractors), including backup infrastructure, to ensure that all devices and services holding ePHI are accounted for and that their security is maintained.
If you are backing up to the cloud, you should ensure that your backup provider is HIPAA compliant, as it is your responsibility to check that all ePHI continues to be properly handled, even after you have passed it on to a third party.
How to reduce HIPAA compliance responsibilities and overheads for your tech teams
Once you’ve implemented your HIPAA-compliant data retention and backup strategies, including encrypted offsite data backups and regular auditing and testing, you should periodically review your data responsibilities. This process should include assessing what data you hold, whether you continue to adhere to the HIPAA security and privacy rules and any new actions you need to take.
Of course, for a comprehensive, detailed view of the legislation and to ensure that you are fully compliant, you need to read and understand the HIPAA document itself in full — no small feat, especially for already busy tech teams.
Additionally, HIPAA and other regulatory data requirements are always being updated and amended and are subject to change and misinterpretation. That’s why it’s important to employ MSPs and leverage platforms that keep up to date with these evolving regulations, taking the work out of remaining compliant.
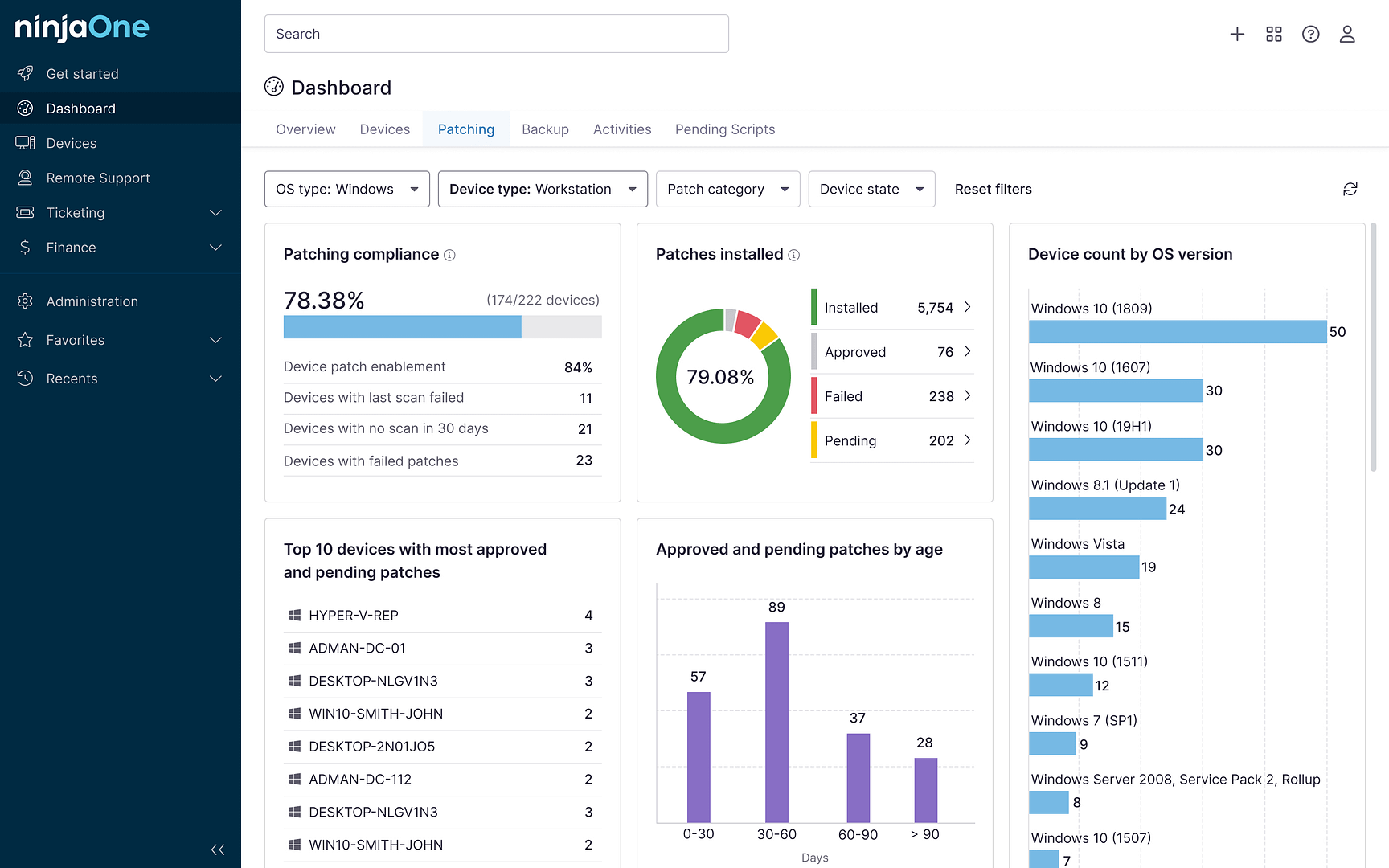
Find out more about how NinjaOne brings together HIPAA compliant remote access, backup, and RMM software into a single IT management platform and how it helps you stay compliant with ever-changing compliance and threat landscapes.